How Allymar Health works with Risk-Bearing Providers
Allymar brings expert advisory services, owned technology and BPaaS offerings and pairs these with industry leading Medicare Advantage technology in one centralized platform. Our health risk-bearing providers benefit from:
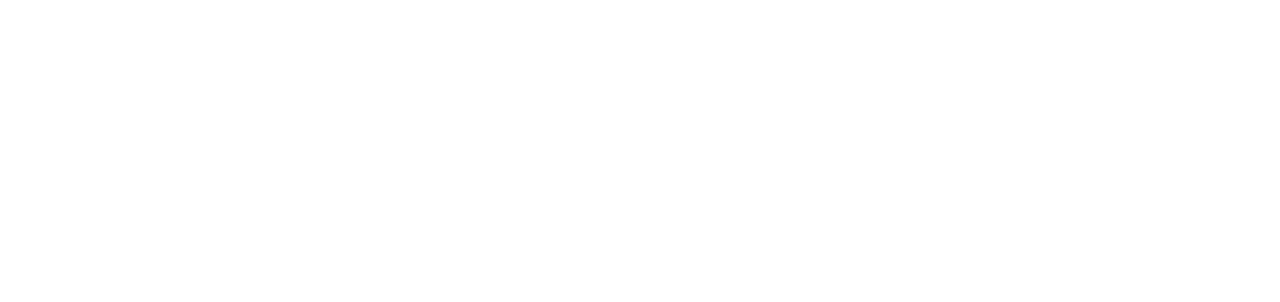
Head-to-head competition
In four (4) recent ‘head-to-head’ comparisons with ‘market-leading’ competitors, our AI outperformed on accuracy and total value.
We have ‘won’ 100% of the ‘head-to-head’ comparisons in the mid and large markets.
*These numbers are based on previous work engagements, and each work engagement will have varying results based on partner and their specific population.
Empowering Clinicians at the point of care with recommendations and detailed reports and insights directly in their EMR
.png)
Take unstructured data from all sources and have that pulled into coding recommendations, care gap opportunities and next steps for patients.
-1705673654.gif)
Our approach
Specifically tailored for risk-bearing providers, the Allymar Health Platform ensures market-leading security and efficiency, all at a price that caters to small and mid-sized health plans.
Unprecedented compliance
Benefit from a fully auditable, traceable system, ensuring maximum compliance with all federal and state regulations.
Member-centric approach
Allymar Health empowers providers and Accountable Care Organizations to prioritize members, ensuring healthy patient outcomes and consistent growth.
.png)
How the Allymar Health AI Platform works

Mrs.Johnson
Understanding the Patient
-
Ingest various structured & unstructured data into the Risk Al Platform.
-
EHR, Claims, Labs, Supplemental Data, etc.
Recapture/Suspect HCCs and Quality Gaps in Care
-
Risk & Quality Reporting Suite
-
Risk Al Platform generates suspect diagnoses and gaps based on machine learning algorithms trained on millions of data.
Point of Care HCC and Gap Closure + Phys. Engagement
-
Provider sees patient in the office and is notified of recapture suspect dx + quality gaps within EHR and captures the diagnoses.
EHR Chart Retrieval
-
EHR Retrieval
-
Fax, Mail, Call Center, Onsite as Needed
Al-Assisted Risk + HEDIS Coding
-
Code charts using Al-assisted coders on the Risk and HEDIS AI Platform.
-
Concurrent Review
Encounter Submissions & Fallout Analysis
-
Submit at 95%+ accuracy with insights into encounter and dx fallout
Financial Projections
-
Estimate incremental financial impact based on payment year
-
RAF accruals & revenue forecasting

*Performance is based on that of the partner and their population and therefore performance may vary.





.png)